The crisis in the NHS has never been greater and resistance is taking new forms as we have seen with the Junior Doctors and Student Nurses. In this piece Mike Downham reflects on his experience as a paediatric doctor in Newcastle in the 1970s to explore what a socialist health service might look like.
Dedication
I would like to register my gratitude to all the patients who have shared their experiences with me over the past 50 years. The ideas put forward in this paper belong to them – the names I have given to some of them do not.
Introduction
There is wide agreement on the left about the urgency of defending the NHS against austerity politics and market-led delivery. But there is little or no discussion about what a socialist health service would look like. Yet surely, on all the fronts of revolutionary struggle, we need to underpin protest and defence with the development of a coherent description of the alternative to capitalism, towards which a gathering mass of people can be drawn, and become convinced that a better future is worth fighting for.
This piece offers some ideas for discussion about the principles on which a socialist health service could be based, how such a service could operate, and about specific pre-revolutionary reforms which we can set our sights on immediately.
The ideas are drawn from my experience of working in the NHS for 20 years, mostly as a children’s doctor in Newcastle upon Tyne, and from a further 30 years’ community activity in Cumbria.
The principles of a socialist NHS
When thinking about the principles on which to base a discussion of what a socialist health service could look like, there are three I would like to suggest as a starting point.
Firstly, the health service must be completely free to everyone, dependent only on need, with no opportunities for anyone to purchase an alternative service.
Secondly, the service will aim to maximise health, giving each individual the chance to enjoy the best possible life (in contrast to the capitalist priority of ensuring a surplus of people well enough to work).
Thirdly, the service will be controlled by the workers who run it together with the people it serves.
When considering these principles it is important to stress that this is more than a return to ‘the spirit of 45’. The original NHS was led by a political elite committed to reforming capitalism, rather than overthrowing it. From the beginning it was heavily contaminated by the vested interests of doctors, who were dragged kicking and screaming into the new NHS in 1948. As early as 1952 the leading principle of the NHS, that it should be free at the point of delivery, was eroded by the introduction of charges for prescriptions and dental treatment. From the beginning people who were able to afford it could purchase private care, though their assumptions that payment gave them better care were not always correct.
After qualifying as a doctor in the 1960s, my first job included first-call responsibility for the patients in the private hospital across the road from the NHS hospital. The benefits private patients received for their money were better food and seclusion in private rooms – otherwise treatment in the two hospitals was identical.
I came to dread calls to see private patients, soon discovering that there weren’t enough nurses to observe the patients adequately in their separate rooms. The Nightingale wards in the NHS hospital worked much better because all patients were visible from the nursing station – and if a patient in trouble wasn’t immediately spotted by the nurses, the patient in the neighbouring bed could be relied on to give a shout down the ward.
Due to the delay in being called to emergencies in the private hospital, I often found myself arriving to find the patient in a life-threatening condition. Resuscitation in the cramped private rooms, less well equipped with oxygen and defibrillators than the NHS wards, was a nightmare. I wasn’t paid for the work in the private hospital – it was just assumed to be part of my NHS job. The consultant I worked under drove a Rolls Royce.
Operating features of a socialist health service
How can these ambitious aims be achieved? As with all organisational aspects of a socialist society, much new thinking and experimentation will be needed. If we feel daunted by the task, we also know from history that once the people collectively take back their birth-right power to organise society, they become inventive to an extent we find hard to imagine in our alienated condition.
The five ideas described below are not intended to be a blueprint. They are ideas which I have had the opportunity to explore in small ways – and attempt to address some of what seem to me to be the worst flaws in the NHS. As such I offer them to the collective ferment.
First idea: Closing the gap between general practice and hospital
During my time as a paediatrician in East Africa in the 1970’s it was not unusual to see a pole slung five feet from the ground between two trees at the entrance to a rural clinic. Women in labour who could walk under the pole without ducking were admitted to the labour ward, on the basis that there is a correlation between short stature and a small pelvis. Women who could not walk under the pole were turned away, the labour ward having neither the space nor the staff to care for them.
How to select patients for special care – for example admission to hospital, as opposed to simple treatment, or no treatment, is a big organisational issue for any health service. It was only gradually through my time as a doctor that I realised how badly this is organised in the NHS.
After leaving the NHS I lived for the next 30 years in a rural community in Cumbria. Over that time neighbours and friends often phoned or came to see me for advice, knowing that I had been a doctor. Usually it was because they were sure there was something seriously wrong with themselves, or with a family member, but had not been referred to hospital by their GP.
I remember Billy, a 12-year-old with swollen neck glands, whose mother had taken him three times to their GP, each time to be reassured that there was nothing serious to worry about. Sally was a 15-year-old with a 3-day history of tummy pain, whose GP told her and her parents to wait and see. Ivy, an elderly (and wise) woman, had seen a TV programme about ovarian cancer and from the symptoms described thought she must have it. But over the previous two months she had failed to get a succession of GPs to take action.
I gave the same advice to all three of these people – go straight to the Accident and Emergency Department of the local hospital. They took my advice, and all three were admitted. Billy proved to have leukaemia, recovering after a long course of treatment. Sally had a badly inflamed appendix removed the same day. Ivy was right – she had ovarian cancer, which had become untreatable. These are not isolated stories. I could tell many similar ones – about unnecessary suffering, and even unnecessary death.
When there is so much talk of the importance of early diagnosis and treatment, why does late referral or non-referral continue to happen? From what I have heard from many patients and doctors, who have shared their experiences, I see four reasons: under-resourced hospitals; power relations between GPs and hospital doctors; the sharp division of responsibility between these two groups of doctors; and an institutionalised lack of respect for patients’ opinions about their illnesses.
As we all know, hospitals, along with all NHS services, have suffered from under-investment for a long time. Particularly disastrous have been the PFI experiment during the Blair years, and frozen NHS budgets under Cameron and May. One result of this is that the junior hospital doctors responsible for deciding whether or not to admit patients referred to them by GPs have become increasingly anxious not to admit patients who might turn out not to have needed admission – an aversion to ‘unnecessary admission’ which they consistently communicate to GPs when they phone to ask for a patient to be admitted. Accordingly, GPs think at least twice before asking for admission, and if in doubt often don’t risk being rejected.
This fear on the part of GPs has been reinforced by their inferior power relationship with hospital doctors, which also goes back a long way. When I was a medical student the general view was that you ended up in General Practice only if you weren’t good enough to become a hospital specialist. Despite strenuous attempts over the years to improve their status and remuneration, many GPs have never fully recovered from this sense of inferiority.
The sharp role delineation between hospital doctors and GPs does not help. The two rarely meet, except in the context of continuing education – usually in the shape of hospital doctors educating GPs. GPs cease to have any say in their patients’ management once they are admitted to hospital, or under specialist care as out-patients. And there is too little opportunity for GPs and hospital doctors to learn together from the mistakes, sometimes fatal, which result from late or non-referral.
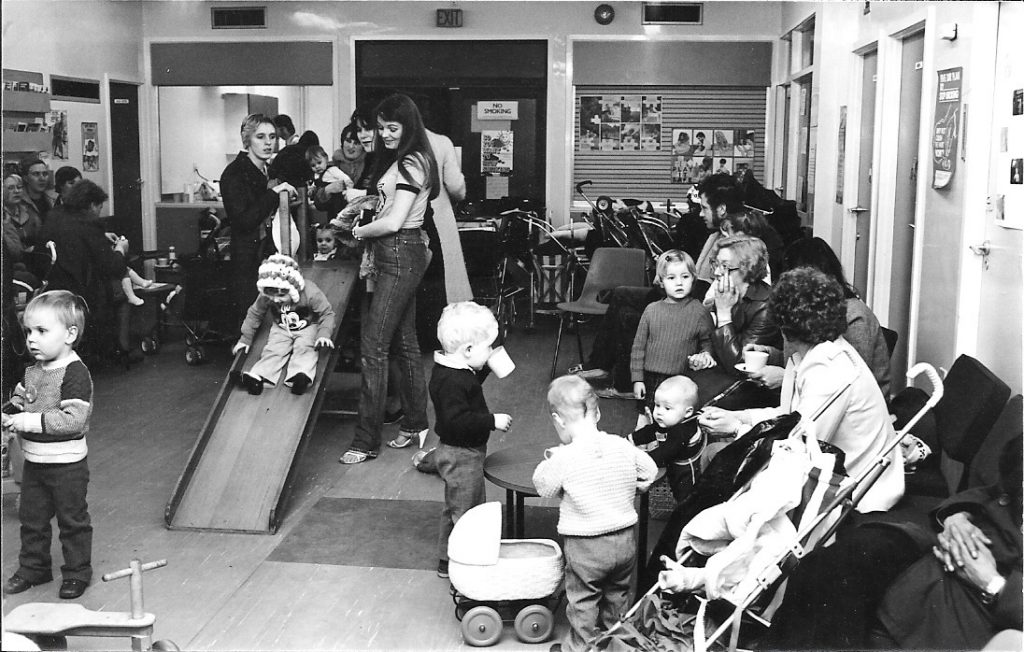
In an attempt to address the power relations between different NHS workers, I had the opportunity to lead an initiative to set up a Riverside Child Health Project (RCHP) in Newcastle upon Tyne in the late 1970’s. We based a team of children’s doctors, health visitors, social workers and community workers in two vacant school classrooms in the desperately deprived west end of the city. We worked as far as we could as equals, sharing the same open-plan office, and cultivating mutual respect through close consultation. We also set up arrangements with all local GPs for regular joint clinics, in which a children’s doctor and the GP would see children together.
The essential feature of these sessions was that they were open, in the sense that parents could bring their child without an appointment, whether they thought she was ill, or weren’t sure whether she was ill, or if they were worried about her development or her behaviour, or if they had family difficulties they wanted to discuss. These sessions were successful from the points of view of both the families who came to them and the GPs, so we extended the system to general practices in the east end of Newcastle.
In a socialist health service it will be essential for power relations to be addressed openly, not only between GPs and hospital doctors, but between all NHS workers, including workers in non-clinical roles whose labour goes into the provision of healthcare.
Second idea: Reducing the workloads of NHS workers
Speaking with junior hospital doctors this year during their protest, I realised that their workloads were not much different from mine 50 years ago.
As a first year doctor in a large London hospital, on alternate days I was on call for new admissions, on top of my responsibility for the 50 patients already in my two wards. On these days we rarely got to the end of our list of tasks before 3.00am, after which we were likely to be called out of bed at least once before getting back to the wards for the next day’s work at 8.00am. We then worked another 12 hours before our night off. Meals on the call days consisted mainly of cornflakes pilfered from the ward kitchen. One in three weekends was ‘off’, which meant getting away about 2.00pm on the Saturday and being back on the ward at 6.00pm on the Sunday. After six months of this I bled three pints from the lining of my stomach and spent the next six weeks in bed on one of my wards.
We knew we were much of the time too exhausted to be good doctors, and that as a result patients were suffering, sometimes even dying unnecessarily. But we felt powerless to change things, conditioned as students to be sycophants, giving ourselves up as burnt offerings to our consultants, the gods we aspired to join. Stepping out of line would have cost us the next six-month job and prejudiced our promotion.
Newly qualified doctors may work fewer hours than we did, but they describe an intense quality of work, driven by the explosion of new technology made available for diagnosis and treatment over the past 50 years.
All in all their work, I think, is every bit as stressful as mine had been, and this is very much a live issue in terms of the Junior Doctors’ dispute with the government.
The government’s attempt to argue that weekend services can be improved without additional resources is a farce, and an insult to the intelligence of the electorate. Their disrespect for the commitment of junior doctors is arrogant in the extreme, and their attempt to discredit them is a cynical and devious excuse for further privatisation. But now there is one big difference from my days.
The mass of junior doctors has learned and organised, and for the first time in history they are identifying themselves as workers, instead of gods. They are standing up for the NHS they believe in, and for their patients whom they care about. Their protest points the way towards a socialist health service, in which all workers will be respected for their contribution and given enough time off for rest and refreshment.
We would do well to start discussing ways of achieving a better balance between the expertise which accumulates through dedication to long hours of work, and the exhaustion which can undermine that expertise and dedication. We can think about more rotation of inevitably challenging front-line responsibilities. We can think about how more support can be given to these workers who hold our lives in their hands – how these crucial services can be better shared between doctors, nurses and other workers – not to achieve revenue savings, but solely to improve the care of patients and the working conditions of those who care for them. If these ideas seem far-fetched, it’s only because we have been beaten over many years into thinking there are no alternatives.
Third idea: Decentralising the delivery of health services
Health issues for people depend heavily on where they live. NHS organisation has always taken too little account of the needs of local people due to its lack of local accountability. In recent years the imbalance of power between Whitehall and local NHS services has become a lever for the centre to impose the same kind of structural adjustment programmes on deficit-spending NHS Trusts, as the EU and IMF have imposed on countries.
People in Cumbria are being subjected to a government-imposed NHS structural adjustment programme called the ‘Success Regime’. The cost-cutting prescriptions coming from Whitehall demonstrate no understanding of the geography of Cumbria, and by failing to recognise the root causes of the deficit compound the problem, threatening a spiralling decline in healthcare for half a million people.
More generally the relationship between poor health – mental and physical – and disadvantage in relation to wealth, employment, housing and services has been clearly established. The poorest areas need a different, more collective, approach to the health of their people, and positive discrimination in the allocation of resources.
The Riverside Child Health Project in Newcastle, described above as an attempt to address the power relations between different NHS workers, also aimed to provide additional resources in the poorest part of the City. The initiative was triggered by research which showed that a disproportionate number of children’s deaths and hospital admissions came from the west-end wards along the bank of the Tyne.
Three years into the project we were able to demonstrate measurable benefits. The improvements in mortality and serious illness rates were small – but this was not surprising, given the massive economic and social problems families continued to face, at a time when capitalism had become rampant in the city. Our experiment was enough to show that a team which included expertise in medicine, preventive health, social work and community development can work well, especially in the way local people developed the confidence to contribute to our strategies, becoming themselves members of the team.
A socialist health service will not achieve health equality overnight. It will need to set up a network of initiatives which discriminate positively for those people who have been most damaged, mentally and physically, by the capitalist system. We need to start discussing ways these locally tailored services can best be delivered, drawing on experience from other countries where attempts have been made. In Cuba, for example, every neighbourhood in Havana has a doctor and a nurse who live in the neighbourhood and have joint responsibility for the neighbourhood’s health.
Fourth idea: Decentralising and democratising the control of health services
Given that health needs vary markedly between different localities, it follows that health services must be locally controlled. Given also that the residents of a locality will understand best what services they need, it must be the local residents who control their services. Here we can see that one of the three basic principles of a socialist health service we started with – that the new service will be controlled by the workers and the people it serves – is not just a socialist idea, but is of material significance in providing the best possible service for all. Here is a test we can usefully apply to all our ideas about how a socialist society could be organised – material difference trumps ideas. Marx grasped this early in his life.
Attempts to democratise the NHS add up to a catalogue of half-hearted or blatantly insincere initiatives, all of which have failed to halt the march of centralisation and dilution of democracy. Local Community Health Councils (CHCs) were set up in 1974 with much rhetoric about a new voice for patients.
As a member of a CHC in Newcastle in the late 1970s I worked alongside other volunteers who were strenuously committed to the cause. We visited hospitals and other services and met monthly. Meetings were long, becoming longer. We never reached the end of the meeting agendas. The meetings became entirely taken up with hefty documents handed down from above, on which we were required to report. With no opportunities to raise the issues fed to me by the impoverished patients I was working with, after two years of getting nowhere I resigned.
In 2003 the Government abolished CHCs without discussion or explanation, to the fury of the many good people who had continued to serve on them with dedication. CHCs were replaced by Public and Patient Involvement Forums (the name admits they had no powers). These were replaced in 2008 by Local Involvement Networks, which in turn were replaced by Healthwatch in 2012 – to give the Government a further opportunity to reduce resources. The frequency of these replacements, with their increasingly vacuous names, testifies to their systemic failure – a failure which was inevitable because all the initiatives were imposed from above by governments whose over-riding priority was to stay in power, not to improve the health of the people.
The central plank of the Riverside Child Health Project (RCHP) in Newcastle was to provide opportunities for small groups of parents to meet informally with a member of the team. In one of these meetings a group of six mothers shared with me their experiences of taking their children to the operating theatre in the local hospital, when they had needed surgery for injuries, or tonsillectomy, or suspected appendicitis. All of them told how their children, most of whom were less than five years old, had been taken from them by a nurse in the corridor outside the anaesthetic room, into which their children were carried screaming. I wrote to a senior anaesthetist about this, and after several rebuffs he accepted the invitation to meet with the group of mothers at the RCHP. Confronted by the mothers, asking him why parents couldn’t stay with their children until they’d been anaesthetised, he agreed to get the policy changed – and it was.
Surely a priority for a socialist health service will be to set up Neighbourhood Health Committees that are well-resourced, fully empowered, and elected from local residents by local residents.
Fifth idea: Reclaiming our bodies
The relationship between doctors and patients in the NHS is an institutionalised contradiction of the fundamental socialist principle that power belongs to the people. This is not to deny that some doctors are better than others at listening to their patients, and at sharing decisions with them about their treatment. But the overall momentum is in the direction of doctors knowing best. We have come to see them as responsible for our health. Genuflective rhetoric from governments and doctors’ organisations about patient empowerment, as with all top-down initiatives, has only served further to embed the power of doctors over patients. The very word ‘patient’, originally meaning one who suffers, has come to signify passivity – a person who is under medical care.
Even our births and our deaths have been appropriated. The Caesarian Section rate in the UK is 25 percent, despite there being no evidence that maternal and new-born death rates improve further once the rate goes above ten percent. In the USA the rate is 33 percent. Death rates of course are not the only relevant measure, but there is also no evidence that non-fatal birth outcomes for mothers and their babies are improved. What in the 1970s and 1980s was a strong women’s movement fighting for less medical intervention in childbirth has evaporated.
The story with death is more encouraging. Terminally ill patients and their families, despite the obvious difficulties for them in organising, have succeeded in getting across to doctors that it is the quality of the life remaining to them which matters, rather than its length. As a result, palliative care, based on decisions led by patients and their families, is rapidly improving, though improvement is restrained by NHS austerity and dangerously dependent on voluntary contributions.
But until we become terminally ill, we continue to see our illnesses as largely or exclusively the territory of doctors. It follows that we seem prepared to endure the extraordinarily harmful side-effects of the treatments which our doctors prescribe, the fall-out from a medical model focussed on cure at all costs, egged on by profit-hungry pharmaceutical companies.
Every illness is uniquely characterised by a particular body’s resilience or vulnerability. Every case of flu, or of appendicitis, presents with subtly different symptoms, and progresses with more or less severity. Every heart attack or stroke is different.
One of the most useful things I was told as a medical student by an enlightened doctor was that the patient is their own best specialist. From this I learned to ask patients early in the consultation what they thought was wrong with them. Nearly always this resulted in the patient giving me useful information in coming to a diagnosis. In the same way, when I began to specialise as a children’s doctor, I learned that parents often have a pretty good hunch about what’s wrong with their child, if only they are given the space and respect to express their opinion. This was particularly important with young children, who can’t localise pain, or explain how they are feeling. The younger the child, the more difficult it can be to distinguish between a serious illness, for example meningitis, and a baby who just happens to be sleepy at the point of consultation. But parents and care-givers usually know.
And so, early on in my time as a doctor, I became aware of the benefit of sharing both diagnostic and treatment decisions with patients, or with the parents of young patients. I began to feel that the NHS gave too little recognition to this potential benefit, and became interested in strategic possibilities for giving patients a larger share in decisions about their illnesses.
Whilst still in the NHS, I conducted a small study with 44 mothers, in which I asked the mothers to keep a dairy of their baby’s symptoms, and their own reactions to them, over an eight-week period. The babies were between 6 and 45 weeks old, and were all first babies. The diaries revealed that these mothers were making almost daily decisions about their baby’s health, usually without seeking medical advice. There was no evidence that the mothers were failing to appreciate the severity of their baby’s symptoms, or failing to seek medical advice when it was needed. This small study reinforced my respect for the ability of the mothers to recognise when their children are ill, even with their first baby.
After quitting my job as a children’s doctor I accepted an invitation to teach orthodox medicine to groups of mature students training to become homeopaths. The invitation was from a well-organised college which delivered an accredited qualification. The aim of including some orthodox medical training in the course was to give students diagnostic skills, particularly for serious conditions which could be life-threatening, and to give them an understanding of the usual course of different illnesses. An outline of the orthodox medical treatment of each illness was included, so that once the students became practising homeopaths they would be able to work in close co-operation with doctors.
I designed a course which took one day a month over two years to teach. It covered the relevant anatomy, physiology, history-taking, physical examination, differential diagnosis, usual course, and orthodox medical management of all illnesses, excluding very rare conditions. The students enjoyed the course, and with minor improvements based on feedback I carried on teaching groups of students for ten years.
Multiple choice assessments showed that nearly all students had understood and retained the information, and were finding it useful in their supervised practice with patients. As I had suspected when a medical student, the five-year course we were given is unnecessarily long for communicating the basics of medicine, given that we only really began to learn about being responsible doctors through supervised practice once we were qualified. The homeopathic students were a special group, highly motivated and most of them previously graduated in teaching, social work, or other university courses. But I emerged from the experience of working with them confident that the most important elements of medical knowledge are straightforward and can be transferred to most people who want to learn.
Later I had the opportunity to do some more research into the way people respond to their symptoms of illness, or the symptoms of their children, and how they use services. In this project I worked alongside some experienced public health researchers. We collected in-depth information from parents of young children and people over 60 years old – two groups likely to be high users of health services. Our findings showed that the people we studied often had an incomplete understanding of the significance of their symptoms, and suggested that training for the general public in recognising and dealing with illnesses should be explored.
On the back of this research, with the help of an experienced health trainer, I designed a course of six two-hour workshops called ‘Dealing with Illnesses’, and offered it to the rural community where I lived. 15 people signed up for the course, all of them women – eleven parents of young children, and four older people. Over the six weeks we covered some common medical emergencies (across all ages), some common childhood illnesses, and some longer-term illnesses. The specific conditions included were chosen by the participants. We used facilitated discussion to share experiences of the symptoms of each condition, and talked about whether and when the participants had gone to the doctor or sought other advice.
Armed with the feed-back from the participants in the ‘Dealing with Illnesses’ workshops I approached a large General Practice to suggest they might try something similar for their patients. The diversity of unconvincing reasons the doctors gave for declining the suggestion (litigation risk, time restraints, room-space restraints …) suggested that the true but unexpressed reason was a reluctance to share power, which goes all the way from the consulting practice to Whitehall and beyond to the pharma corporations.
These experiences have persuaded me that a socialist health service should make training in dealing with illnesses available to everyone. It should start in schools, and be promoted as an adult education option in workplaces and community neighbourhoods. The potential benefits to both people’s health and health service efficiency appear to be huge. And knowledge is power – or at least one of the essential steps towards any transition to socialism.
What is to be done?
As revolutionary socialists we reject the reformist position that a socialist society can evolve over time through progressive reforms. But as Rosa Luxemburg spelled out, ‘the practical daily struggle for reforms, for the amelioration of the conditions of the workers within the framework of the existing social order, and for democratic institutions offers … the only means of engaging in the proletarian class struggle and working in the direction of the final goal – the conquest of political power and the suppression of wage labour.’
What reforms in the NHS should we fight for? I suggest, first, that the current struggle by junior doctors deserves our committed support at every opportunity. This movement, in which doctors are for the first time identifying themselves as workers, and in which the issue (imposition by government of a contract opposed by the workers it applies to) is as relevant to all NHS workers as it is to junior doctors, is fundamentally pre-revolutionary.
Second, I suggest that training in dealing with illnesses could become an immediate focus for radically reforming the NHS. There are a number of features of any potential NHS reform which appear essential from a revolutionary socialist perspective. The first is that that it should be relevant to a large number of people, who are convinced of its possibility. The second is that achievement of the reform would strengthen class-consciousness by taking power back from NHS managers and commissioners and giving greater power to clinical and non-clinical staff working alongside patients and communities. The third is that the reform should aim to put in place a structure of funding and organising health care that puts it on a collision course with the market, and leads to a spiralling of reforms in relation to medical research, provision of drugs and medical equipment, and medical patenting. The fourth is that the reform should be capable of bursting beyond national borders to challenge the global system for provision of health services.
Dealing with illnesses is relevant to everybody. That we are all patients makes it highly achievable. That it is about shifting the balance of power between doctors and patients and challenging the power of Whitehall and the market would strengthen class-consciousness, which in turn would make further reforms more achievable. And there is no reason why it should not spread across borders. A mass movement needs a slogan: ‘Reclaiming Our Bodies’ could be put forward as the slogan for a movement aimed at achieving training in dealing with illnesses for all.
Any struggle for reform risks falling into the trap of seeing the particular reform as an end in itself. To avoid this trap and keep our sights on the goal of a socialist society, it’s useful from the start to identify in broad terms further changes that could be brought about by a mass movement challenging the current provision of healthcare. Areas which such reforms could focus on include the provision of new NHS workers, rooted in communities, as the first point of contact for people seeking advice about illness or health. Whereas a neoliberal version of this would consist of stripping resources out from GP practices and making pharmacies do more clinical work, a socialist version could consist of training up and developing workers based in their local neighbourhoods and elected by, and accountable to, the neighbourhood’s residents. Another step could be the establishment of committees or collective bodies born out of struggle that are properly resourced and can act as organs for the planning and delivery of health services relevant to their neighbourhood. These would become the cells of a collective socialist NHS that would be networked across communities, specialisms and ultimately borders.
When we look with dismay at the poor physical and mental health of people in a country like Britain, and at the failure in many respects of the NHS to improve their health, we can take heart from recognising that a large proportion of current ill health is the product of a capitalist society. And we can look towards the time when neoliberal politics, unequal power relations, unpleasant working conditions and profit-focussed drug production – all the things which currently underpin ill health – will be peeled away in the socialist revolution.
Mike Downham is a retired paediatrician who worked from the 1960s to the early 1980s in Newcastle and Zambia. On leaving the NHS he has been an organic farmer and community activist for the past 30 years. This piece is his first written publication.


















Reblogged this on Niallist's Weblog.
This is a really brilliant article. It is brilliant to have something that isn’t just about defending the NHS but going further.